
Pharmacy Choice White Paper
PHARMACY CHOICE
In workers’ compensation, injured workers are permitted to fill their prescriptions at their pharmacy of choice in most states. An injured worker may be able to choose their pharmacy and physician without any limitations throughout their recovery journey. As pharmacy choice is handled on a state-by-state basis, there are instances where an injured worker cannot choose their pharmacy but could select their physician and vice versa. Providing injured workers with the ability to pick their medical providers might seem simple, but answers can remain complex throughout the states.
Statutes, regulations, judicial precedent, and general protocols play a factor in determining if an injured worker retains the ability to choose their pharmacy. Arkansas, Iowa, Louisiana, Missouri, and New Jersey established the employer’s right to select where the injured worker will go for pharmacy services. Meanwhile, most states generally allow injured workers to receive prescription services from their pharmacy of choice. Of these states, only Florida, Maine, New Hampshire, and Texas guarantee this right to choose by statute.
“Choice” Fluctuates
While Florida, Maine, New Hampshire & Texas lay out statutory precedent for an injured worker’s right to choose pharmaceutical services, most states will either attempt to interpret existing statutes, direct state agencies to create rules, or require the courts to intervene as seen in Louisiana & Kentucky.
The definition of “choice” fluctuates in each state. Some regulators view choice as where an injured worker holds the ultimate right to choose their medical service providers. Whereas other states may see choice as a selection within an employer’s designated network, such as a preferred provider plan (PPN), managed care organization (MCO), or preferred provider organization (PPO). Caveats often present themselves when it comes to pharmacy choice in workers’ compensation. For example, while providing for pharmacy choice, Pennsylvania requires injured workers to go through an employer’s chosen medical providers for the first 90 days of treatment (Title 77 Sec 306) before utilizing a pharmacy/medical provider of their choosing.
States may permit employers and their designated insurance network plans to redirect the care of injured workers, a term dubbed direction of care (DOC). This precedent is exemplified in Arizona, Nevada, and West Virginia, where self-insured employers may redirect an injured worker’s medical care and subsequently choose their pharmacy for them. Similar actions are seen in Connecticut, where MCO’s may direct injured workers to a pharmacy within a network, and in North Carolina, as conditions of authorization are primarily handled by the employer/carrier.
A more recent example of directing care occurred in New York in 2022. The Workers’ Compensation Commission (NYWCB) approved rule 440.8(c), a measure dictating that injured workers must receive prescription care from in-network pharmacies selected by their insurance carrier or PBM. As written, the rule abolishes an injured worker’s ability to choose where they receive prescription care. Previously the NYWCB gave the option of directing care to PBMs and insurance carriers, providing injured workers with some flexibility in pharmacy choice.
Throughout the workers’ compensation system, states may grant an injured worker the ability to choose their pharmacy but not their physician. Alabama, Idaho, Iowa, and Kansas give employers the right to select the injured worker’s physician while simultaneously allowing injured workers to choose their pharmacy if they need prescription services. Meanwhile, Louisiana, New York, New Mexico, Michigan, and Minnesota will generally enable injured workers to choose their physician and deny them the choice of pharmacy.
For and Against Pharmacy Choice
Pharmacy choice to most, is regarded as the injured worker’s ability to select their pharmacy without any barriers or obstruction. Advocates for pharmacy choice argue that permitting injured workers to select their pharmacy will provide confidence in their treatment and overall recovery. Supporters of choice also see it as essential for injured workers to receive care separate from their employer’s providers to avoid conflicts of interest that could potentially jeopardize recovery efforts. Those opposed to pharmacy choice regard cost and treatment outcomes as ultimate factors for restricting pharmacy choice.
If injured workers choose outside of contracted pharmacy networks or accept physician-dispensed drugs, opponents say this will ultimately increase the price of drugs and place financial strain on the workers’ compensation system. Those against pharmacy choice contend that smaller pharmacies and those out of network do not hold the same bargaining power as pharmacy benefit managers (PBMs) and network plans with drug manufacturers, therefore indirectly increasing drug costs. Cynics of choice also question the quality of treatment, arguing that since PBMs and network pharmacies
are more conditioned to the workers’ compensation system, their frequent familiarity enables them to
better adhere to state formulary requirements and treatment guidelines.
Research Findings
Multiple analyses demonstrate that patients experience greater satisfaction and treatment compliance when actively participating in their care.(i) Evidence from the Journal of Occupational Rehabilitation suggests that injured workers innately hold a lack of trust with their employer to act in their best interest in the return-to-work process as they undergo treatment.(ii) Findings also conclude that establishing a connection with your providers is likely to strengthen treatment adherence and overall recovery. Studies from the Journal of Chiropractic Medicine, the Industrial and Labor Relations Review, and the Journal of Occupational and Environmental Medicine show that injured workers with a positive provider relationship demonstrated greater understanding of treatment rationale, enhanced treatment compliance and improved expectations that care needs will be met.(iii),(iv),(v) An international literature review of treatment and provider choice in worker injury rehabilitation analyzing 19 studies between 2007 and 2018, 10 of which were from the U.S., determined that in all “choice of provider or treatment generated more positive outcomes for workers.”(vi) Choice advocates believe injured workers will put more effort towards their recovery if they can freely choose their pharmacy for their prescription treatment. According to supporters of choice, necessitating an injured worker to utilize a provider of their employer’s choice may not give them complete confidence that their medical needs will be fully met.
Prior research findings relating to provider choice in workers’ compensation show slightly higher medical cost associated with states where workers were able to choose their medical providers.(vii) However, in the last decade, with the exception of particular severe injuries, recent estimates from Workers’ Compensation Research Institute (WCRI) imply that there’s no difference in average medical costs between states where employers chose providers for injured workers and states where injured workers chose their providers.(viii) This result applies to the most common injuries. Research outcomes suggest that there is no significant cost difference in indemnity benefits between states where employers choose and those states that provide for injured workers choice. When observing lost time due to injury, the percentage of claims with more than seven days of lost time were nearly identical between employer choice and injured worker choice states. Researchers believe “more worker control of provider choice may lead to better medical decision-making, perhaps because of more trust between the patient and the treating provider, lower likelihood of disputes about care and - when workers choose providers familiar with their medical history and conditions better information about the worker that leads to better and more effective treatment decisions.”(viii)
Where Pharmacy Choice Stands in Workers’ Compensation
Current evidence validates an injured worker’s ability to choose their medical provider, including their pharmacy, can benefit treatment adherence, improve recovery and lead to successful return to work outcomes while at the same time not affecting costs. Although some states may claim that limiting
choice is effective in controlling costs and improving treatment quality, the Department of Labor (DOL) refute such arguments in recent studies seeing that “it is not clear that many of these efforts (to restrict provider choice) have succeeded in achieving either goal” of controlling costs or improving treatment standards.(ix) Nevertheless, prior study on the subject does, at times, exhibit a slight tendency for states providing choice to experience increased costs for certain patient populations. However, with expenditure concerns settled by the past decade of research, states may want to more comprehensively evaluate how patient choice impacts the system. Factors including patient outcomes, adherence, satisfaction, and treatment compliance should weigh into the pharmacy choice debate moving forward to accurately assess the full effects of choice in workers’ compensation.
PHARMACY CHOICE BY STATE
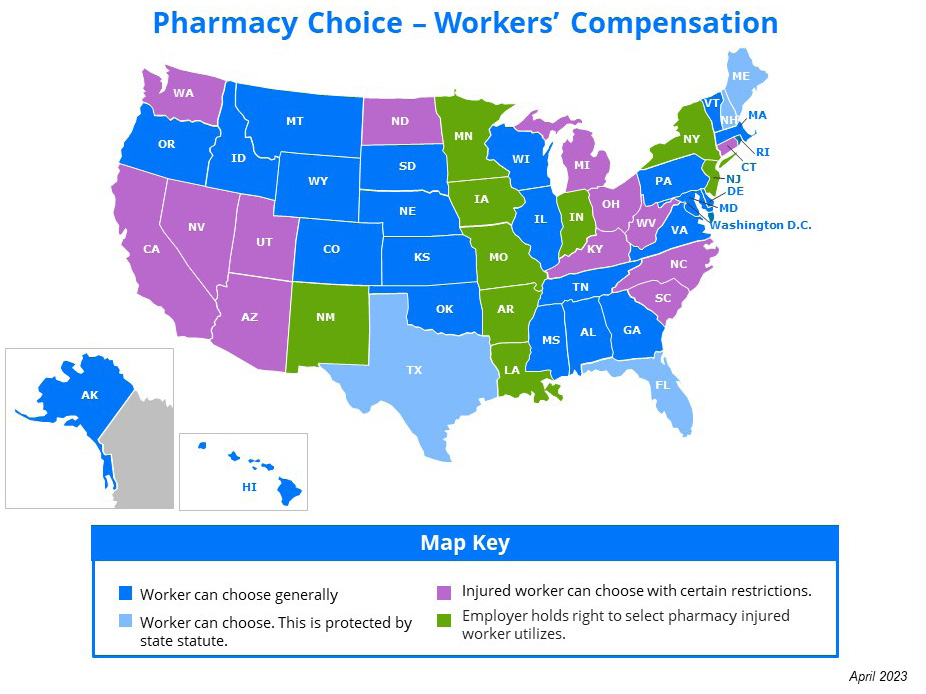
- Alabama – Worker can choose generally.
- Alaska – Worker can choose generally.
- Arizona - Injured worker can choose with certain restrictions. Self-insured entities can direct care.
- Arkansas – Employer holds right to select pharmacy injured worker utilizes.
- California – Injured worker can choose with certain restrictions.
- Colorado - Worker can choose generally.
- Connecticut - Injured worker can choose with certain restrictions.
- Delaware - Worker can choose generally.
- Florida - Worker can choose. This is protected by state statute.
- Georgia - Worker can choose generally.
- Hawaii – Worker is entitled to choose their pharmacy.
- Idaho - Worker is entitled to choose their pharmacy.
- Illinois – Worker has the right to choose their pharmacy.
- Indiana - Employer holds right to select pharmacy injured worker utilizes.
- Iowa - Employer holds right to select pharmacy injured worker utilizes.
- Kansas - Worker can choose generally.
- Kentucky - Injured worker can choose with certain restrictions.
- Louisiana - Employer holds right to select pharmacy injured worker utilizes.
- Maine - Worker can choose. This is protected by state statute.
- Maryland - Worker has the right to choose their pharmacy.
- Massachusetts - Worker has the right to choose their pharmacy.
- Michigan - Employer holds right to select pharmacy injured worker utilizes.
- Minnesota - Employer holds right to select pharmacy injured worker utilizes.
- Mississippi - Worker can choose generally.
- Missouri - Employer holds right to select pharmacy injured worker utilizes.
- Montana - Worker can choose generally. However, state fund requires use of in network pharmacies.
- Nebraska - Worker can choose generally.
- Nevada - Worker can choose generally. However, if employer operates managed care plan or is self-insured, employer may direct pharmacy care.
- New Hampshire - Worker can choose. This is protected by state statute.
- New Jersey - Employer holds right to select pharmacy injured worker utilizes.
- New Mexico - Employer holds right to select pharmacy injured worker utilizes.
- New York - Employer holds right to select pharmacy injured worker utilizes.
- North Carolina – Injured worker can choose with certain restrictions. Direction of care may apply.
- North Dakota - Injured worker can choose within network generally.
- Ohio - Worker has the right to choose their pharmacy. Must be registered with BWC.
- Oklahoma - Worker has the right to choose their pharmacy.
- Oregon - Worker has the right to choose their pharmacy.
- Pennsylvania - Worker has the right to choose their pharmacy.
- Rhode Island - Worker has the right to choose their pharmacy.
- South Carolina - Worker has the right to choose their pharmacy. Provider may direct care if they so choose.
- South Dakota - Worker has the right to choose their pharmacy.
- Tennessee - Worker has the right to choose their pharmacy.
- Texas - Worker has the right to choose their pharmacy.
- Utah - Injured worker can choose with certain restrictions.
- Vermont - Worker has the right to choose their pharmacy.
- Virginia - Worker has the right to choose their pharmacy.
- Washington - Injured worker can choose with restrictions.
- West Virginia - Injured worker can choose with certain restrictions. MCO’s and Self-Insured Employers may direct care.
- Wisconsin - Worker has the right to choose their pharmacy.
- Wyoming - Worker has the right to choose their pharmacy.
WORKS CITED
i. Martin L., Williams S., Haskard K & DiMatteo R. (2005, September 13). The challenge of patient adherence - Therapeutics and Clinical Risk Management Journal. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1661624/.
ii. White C., Green R., Ferguson S, Anderson S, Howe C, Sun J. & Buys N. (2019, January 22). The Influence of Social Support and Social Integration Factors on return to Work Outcomes for Individuals with Work-Related Injuries: A Systematic Review – Journal of Occupational Rehabilitation. Retrieved from: https://link.springer.com/article/10.1007/s10926-018-09826-x.
iii. Gilkey D. , Caddy L. , Keefe T. , Wahl G. , Mobus R. , Enebo B. , Duvall K. , & Griffiths K. (2008, December). Colorado workers’ compensation : medical vs chiropractic costs for the treatment of low back pain - Journal of Chiropractic Medicine. Retrieved from: https://www.sciencedirect.com/science/article/abs/pii/S1556370708000965
iv. Neumark D., Barth P., & Victor R. (2007, October). The impact of provider choice on workers’ compensation costs and outcomes. Industrial and Labor Relations Review. Retrieved from: https://journals.sagepub.com/doi/10.1177/001979390706100107
v. Pourat N. , Kominski G. , Roby D. , & Cameron M. (2007, November). Satisfaction with care and perceptions of quality among injured workers in California’s workers’ compensation system - Journal of Occupational and Environmental Medicine. Retrieved from: https://doi.org/10.1097/JOM.0b013e3181566b5e
vi. Anderson O., McLennan V. & Randall C. (2021, July 1). Treatment and provider choice in worker injury rehabilitation: a systematic literature review – Journal of Vocational Rehabilitation. Retrieved from: https://content.iospress.com/articles/journal-of-vocational-rehabilitation/jvr211171
vii. Victor R., Barth P, Neumark D. (2005, November 1). The Impact of Provider Choice on Workers’ Compensation Costs and Outcomes – Workers’ Compensation Research Institute. Retrieved from: https://www.wcrinet.org/reports/the-impact-of-provider-choice-on-workers-compensation-costs-and-outcomes.
viii. Neumark D & Savych B. (2017, April 26). The Effects of Provider Choice Policies on Workers’ Compensation Costs - Workers’ Compensation Research Institute. Retrieved from: https://www.wcrinet.org/reports/the-effects-of-provider-choice-policies-on-workers-compensation-costs.
ix. US Department of Labor. (2016, September 23). Does The Workers’ Compensation System Fulfill Its Obligations to Injured Workers? Retrieved from: https://www.dol.gov/sites/dolgov/files/OASP/files/WorkersCompensationSystemReport.pdf.

