
Pharmacy Choice White Paper
Overview
Telemedicine, also known as telehealth and vice versa is gaining a significant presence in the workers’ compensation industry. Due to the pandemic, numerous healthcare clinicians turned to the virtual world to accommodate their patients’ wide range of medical needs to compensate for less physical access to providers. Originally, telemedicine became most prominent for mental health services. With the recent rise of remote work and society’s swift adaptability to technology, regular utilization of the practice is becoming a new normal in nearly every healthcare sector. According to the American Hospital Association, 76 percent of U.S. hospitals say they are already equipped for routine telemedicine usage.i
Even as the pandemic winds down and vaccinations continue to make their way, telemedicine is likely here to stay. Americans already have experience with virtual healthcare visits, particularly military veterans. The US Department of Veteran’s Affairs offered telemedicine services as early as 2003. Today with more Americans returning to work and resuming typical day-to-day activities, schedules are becoming congested once again.
Telemedicine holds the capability to redefine healthcare with benefits such as accommodating busy schedules for both providers and patients, increasing safety from illness exposure, and significant cost reductions in travel and meeting time. Though, at the same time, some say telemedicine remains a developing service. Skeptics claim that in-person services are still necessary to best guarantee quality of care and ensure a thorough examination from healthcare providers. Numerous doctors and nurses say that telemedicine does not account for seeing someone’s movements or skin characteristics up close, potentially leading to a missed diagnosis. Some are also concerned about internet privacy regarding medical information being discussed. Healthcare professionals remain mixed on telemedicine, specifically audio-only services. Many in the healthcare industry say that those without video telemedicine or in-person appointments are less likely to come back for follow-up visits.ii Due to these findings, a significant number of healthcare professionals opt for a hybrid approach to allow for flexibility and safeguard the quality of service simultaneously.
Although telemedicine may not be able to treat severe injuries, the technology does have the capability to treat the most common workplace injuries, from strains and sprains to cuts and scrapes. Some major companies suggest that technology be on hand at large work sites to allow injured workers to receive care and guidance immediately as injuries arise. Industry leaders believe health hubs onsite at work via electronic platforms could more efficiently determine injury severity and dictate the course of action if necessary for treatment.
While there are benefits and drawbacks to telemedicine, its popularity cannot be denied. From March to April of 2020, telemedicine appointments increased 91 percent in workers’ compensation claims.iii In response to demand for virtual visits, workers’ compensation providers invested heavily in new technology systems, with 35 percent citingiv that telemedicine will have an immense impact on the industry in the next 5-10 years. 89 percent of healthcare industry leaders say they are now investing substantially in telemedicine capabilities.v
Investment in the technology seems to make sense for the workers’ compensation industry as cost reductions for providers and employers can be quite significant, with many seeing decreases of around 50% in certain services . There is also the benefit of younger generations wanting more flexibility with accessing medical services. Over half of Millennials and Gen-Zers prefer to replace their primary physicians with a network of telemedicine providers.vi
Telemedicine’s Underserved Populations
While telemedicine is an obvious option for those with the internet, the service may not be fully accessible to all the population due to lagging broadband networks in rural or underserved areas of the country. The Federal Communications Commission reports that 19 million Americans cannot access the internet as of 2021.vii Even worse, the FCC estimates that 44 million households do not have a standard broadband connection either because they cannot gain access or it’s simply not affordable.viii
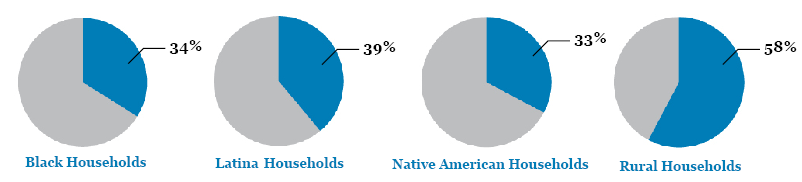
Digital gaps tend to affect minority populations as 34 percent of Black households, 39 percent of Latina households and 33 percent of Native American households have no broadband subscriptions. Rural Americans suffer from lagging connectivity as well, with 58 percent reporting that limited access to high-speed internet is a problem in their community.ix
There is also a divide in age on telemedicine practices. Over one-third of those above the age of 65 report significant concerns with their ability to use telemedicine technology.x Altogether 41 percent of Medicare beneficiaries lacked access to a computer with high-speed internet access, and many also reported not having a smartphone with a wireless data plan.xi
Older adults tend to need more medical attention than other populations, with the 55+ age demographic accounting for over half of total health spending in the country. A rapid switch to telemedicine may hurt more than help older Americans and minority communities unless broadband is extended to these underserved populations.xii
State Access
To make way for telemedicine, nearly all states proposed legislation related to the practice this year. Well over 1,000 bills related to telehealth and telemedicine were filed in 2021 alone. Telemedicine-related bills were not exclusively identical as state legislators grappled with a long list of issues unique to their state, such as licensing procedures, technological hiccups, clarification of definitions, and scope of insurance coverage. States like Arizona, Delaware, Kentucky & Montana fully passed omnibus bills related to telemedicine covering a range of issues within each state’s health system. Meanwhile, states like Georgia, Indiana, Louisiana, Maryland, Minnesota, Oregon, Virginia made legislative clarifications or expanded on their definition of telemedicine in attempts to simplify existing statutes.
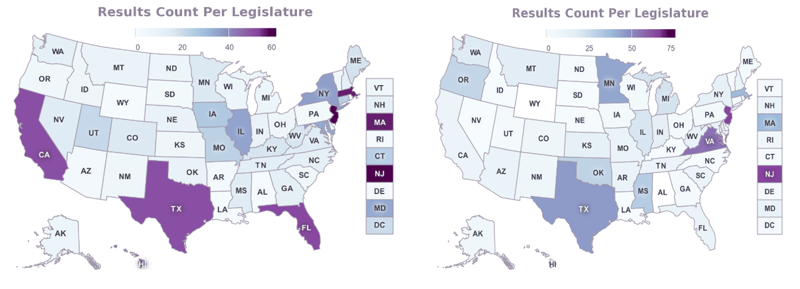
Telehealth related bills (left) and Telemedicine related bills (right) filed in 2021 provided by Fiscal Note
Colorado, Oklahoma & South Dakota fully passed tech-neutral definition legislation in the 2021 session. Technological neutrality involves not being reliant on specific software or technological outlets to operate. A tech-neutral telemedicine partner permits streamlined integration with existing healthcare systems’ processes and technical preferences allowing for greater flexibility. For example, South Dakota’s bill (SB96) eliminated the state’s prohibition on audio-only, email, and text communication for telemedicine.
With the switch to virtual visits, many providers called on their state legislatures to ensure pay parity for telemedicine appointments, guaranteeing online appointments are reimbursed the same as in-person visits. While most states do not enforce pay parity for telemedicine, 24 states do. However, pay parity can depend on the type of services being delivered. As an example, Alaska, Illinois, and Massachusetts only require pay parity for mental health services.
In workers’ compensation, all states except for Arkansas allow telemedicine to be used in some capacity. Before 2020 less than half of states allowed for telemedicine in workers’ compensation. Since the pandemic, over half of US states either added a telemedicine option or expanded their usage for worker’s injuries.xiii More than 30 states included updated procedural codes for telehealth services in their workers’ compensation fee schedules.xiv
In 2021, 26 states (Arizona, Arkansas, California, Connecticut, Colorado, Delaware, Georgia, Indiana, Kentucky, Louisiana, Maine, Maryland, Minnesota, Montana, New York, North Dakota, Nevada, Oklahoma, Oregon, Rhode Island, South Dakota, Tennessee, Texas, Virginia, Washington, West Virginia) officially enacted significant legislation expanding telehealth services and or clarifying definitions.
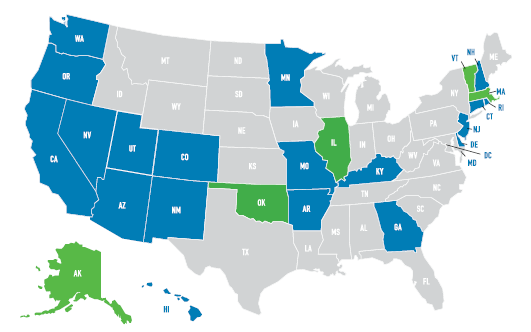
Source: Mannett Health (Implemented Pay Parity, Implemented with Caveats)Conclusion
Overall, telemedicine dominated legislative circles in the 2021 session and should continue to do so into 2022 and beyond. Virtual care is likely to develop into the norm and to more healthcare sectors. With the expansion of telemedicine, state authorities and regulators may need to be up to date on their statutes to ensure coverage and accessibility in their areas as issues emerge. The technology could become mainstream in workers’ compensation and solve longtime problems ranging from time lost to recovery efficiency. However, it could also experience its own set of issues without proper implementation.
Legislators and regulatory authorities used various tools to ensure their state’s residents could access health services limited by the pandemic. From passing legislation to issuing emergency orders, the expansion of telehealth is seen as a developing success of the U.S. healthcare system. Telemedicine’s potential is yet to see its limits. However, private-public sector partnership and cooperation are necessary to deliver critical services to unlock its full potential. Investments in broadband and the loosening administrative red tape from the states may be needed for telemedicine to be comprehensively delivered on a nationwide basis.
SOURCES
i. American Hospital Association (AHA). (2021). Fact Sheet: Telehealth. Retrieved from: https://www.aha.org/factsheet/telehealth
ii. Nogushi Y. (2021, November 23). Voice Only Health May Go Away with Pandemic Rules Expiring -NPR. Retrieved from: www.npr.org/sections/health-shots/2021/11/23/1056612250/voice-only-telehealth-might-go-away-with-pandemic-rules-set-to-expire
iii. Hatamian S. (2020, December 29). 5 Keys to Sustaining Effective Workers’ Compensation Telehealth Usage Beyond the Pandemic – Risk & Insurance Journal. Retrieved from:
riskandinsurance.com/5-keys-to-sustaining-effective-wc-telehealth-usage-beyond-the-pandemic
iv. Enlyte-Mitchell. (2021, April). Technology Most Adopted by Workers’ Compensation Organizations During Covid-19 Pandemic. Retrieved from: https://www.mitchell.com/news/mitchell-survey-identifies-technologies-most-adopted-workers-compensation-organizations-during
v. Jercich K. (2021, May 5). Majority of healthcare decision makers prioritize virtual care delivery – HealthcareITNews.). Retrieved from: healthcareitnews.com/news/majority-healthcare-decision-makers-prioritize-virtual-care-delivery-says-philips-report
vi. Tereshchenko N. (2021, August 8). Benefits and Growth of Telemedicine in Workers’ Compensation – Medcor. Retrieved from: medcor.com/2021/08/08/the-benefits-growth-of-telemedicine-in-workers-compensation
vii. Federal Communications Commission (FCC). (2012, August 21). Eight Broadband Progress Report. Retrieved from: fcc.gov/reports-research/reports/broadband-progress-reports/eighth-broadband-progress-report#:~:text=Notwithstanding%20this%20progress%2C%20the%20Report,broadband%20service%20at%20threshold%20speeds
viii. Federal Communications Commission (FCC). (2018, December 31). Internet Access Services: Industry Analysis Division Office of Economics and Analytics September 2020. Retrieved from: FCC.
ix. Anderson M. (2018, March 10). About a quarter of rural Americans say access to high speed internet is a problem – Pew Research Center. Retrieved from: pewresearch.org/fact-tank/2018/09/10/about-a-quarter-of-rural-americans-say-access-to-high-speed-internet-is-a-major-problem
x. George J. (2020 August 4). Telehealth Boom Misses Older Adults – MedPageToday. Retrieved from: medpagetoday.com/practicemanagement/telehealth/87901
xi. Lam K., Lu. A & Shi Y. (2020, August 3). Assessing Telemedicine Unreadiness Among Older Adults in the United States During the Covid-19 Pandemic – JAMA Network. Retrieved from jamanetwork.com/journals/jamainternalmedicine/fullarticle/2768772
xii. Ortaliza J., McGough M., Wager E. & Claxton G. (2021, November 12). How do health expenditures vary across the population - Peterson KFF. Retrieved from: healthsystemtracker.org/chart-collection/health-expenditures-vary-across-population
xiii. AmTrust Financial. (2021). Telehealth & Workers’ Compensation: Benefits & Recovery Outcomes. Retrieved from: amtrustfinancial.com/blog/small-business/telehealth-and-workers-comp
xiv. Powell M. (2021, April 2). Workers’ Compensation Research Institute: Nearly Every State Pays for Telehealth Services, Many in Response to Covid-19. Retrieved from: workcompcentral.com/news/article/id/63d66965f58c52f9caeb8ed8cdd2f8461ca3667a

